Dr. Danesh D. Chinoy is a leading Health and Wellness Coach, Sports Physiotherapist and Psychologist. He is dedicated to helping all to heal holistically and remain fighting fit for life. Providing eye-opening and ground-breaking insights into Wellness, Dr. Chinoy’s two-decades’ rich expertise has won him innumerable awards, nationally and globally. His mission is to empower you to reach your highest levels of wellness/fitness. You can connect with Dr. Chinoy at: daneshchinoy@gmail.com .
 About 8 in 10 people have one or more bouts of Lower Back Pain. Most often, it is not due to a serious disease or major back problem, and the exact cause of the pain is not clear. This is called non-specific Lower Back Pain. The usual advice is to keep active and do normal activities as much as possible. Painkillers can help until the pain eases. In most cases, the pain disappears within a few weeks but may recur. Persistent (chronic) pain develops in some cases and further specific treatment may then be needed.
About 8 in 10 people have one or more bouts of Lower Back Pain. Most often, it is not due to a serious disease or major back problem, and the exact cause of the pain is not clear. This is called non-specific Lower Back Pain. The usual advice is to keep active and do normal activities as much as possible. Painkillers can help until the pain eases. In most cases, the pain disappears within a few weeks but may recur. Persistent (chronic) pain develops in some cases and further specific treatment may then be needed.
The lower back is also called the lumbosacral area of the back. Most of the lower back is made of muscles that attach to, and surround, the spine. Many people confuse the spine with the spinal cord. The spine is made up of many bones called vertebrae, which are roughly circular in shape. Between each vertebra is a disc. These discs between the vertebrae are a combination of a strong fibrous outer layer and a softer, gel-like centre. The discs act as shock absorbers, allowing the spine to be flexible. Strong ligaments also attach to nearby (adjacent) vertebrae to give extra support and strength to the spine. The various muscles that are attached to the spine enable the spine to bend and move in various ways.
The spinal cord contains the nerve pathways to and from the brain, and is contained and protected within the spine. Nerves from the spinal cord come out from between the vertebrae to take and receive messages to various parts of the body.
The majority of cases of sudden-onset (acute) low back pain are classed as non-specific. This is the type of back pain that most people will have at some point in their lives. It is called non-specific because it is usually not clear what exactly is causing the pain. In other words, there is no specific problem or disease that can be identified as the cause. The range of pain can still vary from mild to severe.
Nerve-root pain – often called sciatica – occurs in about 1 of every 20 acute low back pain patients. Nerve root pain means that a nerve coming out from the spinal cord (the root of the nerve) is irritated or pressed on. (Many people call this a trapped nerve.) You feel pain along the course of the nerve. Therefore, you typically feel pain down your leg, extending sometimes, even up to the calf or foot. This pain, in the leg or foot, is often worse than the pain in the back. The irritation or pressure on the nerve may also cause pins and needles, numbness or weakness in parts of the buttock, leg or foot.
About 9 in 10 cases of nerve-root back pain are due to a prolapsed disc – generally called a slipped disc. A disc does not actually slip. What happens is that the inner soft part of the disc bulges out (prolapses) through a weakness in the outer hard part of the disc. The prolapsed part of the disc presses on a nerve nearby.
There may be many other causes of pain that can only be evaluated upon examination and investigations but most people who develop lower back pain that comes on suddenly (acutely), have non-specific lower back pain. If there are no other associated symptoms and the pain is not too bad, many people are confident to just ‘get on with it’ and treat it themselves – and indeed, most do recover quickly.
However, if in doubt, or if you have any of the undermentioned symptoms, please do consult your physiotherapist:
- Pain that develops gradually and slowly, gets worse and worse over days or weeks.
- Constant back pain that is not eased by lying down or resting.
- Pain that travels to the chest, or is higher in the back behind the chest.
- Weakness of any muscles in legs.
- Lack of feeling (numbness) in any part of your bottom or leg.
- Pain which is worse in the second half of the night or after waking.
- Stiffness, in addition to pain, of the back muscles in the morning after getting up from bed that lasts for more than 30 minutes.
- Numbness around the back passage – the saddle area.
- Bladder symptoms such as loss of bladder sensation; loss of bladder control, incontinence, loss of sensation when urinating.
- Incontinence of stools.
- Back pain following major trauma such as an accident.
- General symptoms, such as high temperature, unexplained weight loss, etc.
Investigation techniques like X-rays, MRI scans or even blood tests may be advised in certain situations. This is mainly if there are symptoms, or signs during examination, to suggest that there may be a serious underlying cause for the back pain.
The following undermentioned advice should help in a sudden-onset (acute) bout of nonspecific low back pain:
Keep Active: Continue with normal daily activities as much as possible. This may not be possible at first if the pain is very bad. However, move around as soon as you are able, and get back into normal activities as soon as you can. As a rule, don’t do anything that causes a lot of pain. However, you will have to accept some discomfort when you are trying to keep active. Setting a new goal each day may be a good idea. For example, walking around the house on one day, a walk to the shop next day, etc.
Sleep Comfortably: Sleep in the most naturally comfortable position on whatever is the most comfortable surface for you.
Get Back To Work: If you have a job, aim to get back to work as soon as possible. Returning to work often helps to relieve pain by getting back to a normal pattern of activity and providing a distraction from the pain.
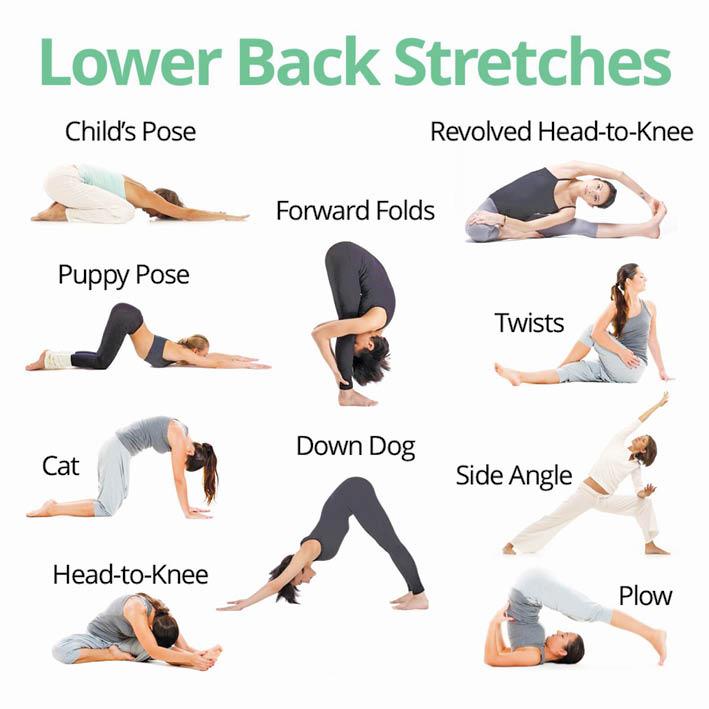
Stretches And Exercises: Back stretching and strengthening exercises will go a long way in keeping your spine pain free.
Get Moving: In the past, one was advised to rest until the pain eases. It is now known that this was wrong. The evidence from research trials is that you are likely to recover more quickly by getting moving again as soon as possible. Also, you are less likely to develop persistent (chronic) back pain if you keep active when you have back pain rather than resting a lot.
Heat Therapy: Heat – such as a hot bath, may help to ease pain
Manual Therapy: Typically, this includes few sessions of massage, spinal mobilization/manipulation from an expert physiotherapist.
- The Healing Power Of ‘Shinrin-Yoku’ (Forest Bathing) - 28 December2024
- The Incomparable Health Benefits Of Plant-Based Diet - 30 November2024
- The Role Of Physiotherapy In Mental Health: A Holistic Approach - 28 September2024
