 As we journey through life, our bodies undergo countless transformations. Amidst the whirlwind of changes, there’s one silent shift that often goes unnoticed until it makes its presence known: the gradual weakening of our bones. Yes, as the years pass, our once sturdy skeletal framework can become fragile, leaving us vulnerable to fractures and osteoporosis. But armed with knowledge and proactive steps, you can defy the odds and maintain robust bone health well into your golden years.
As we journey through life, our bodies undergo countless transformations. Amidst the whirlwind of changes, there’s one silent shift that often goes unnoticed until it makes its presence known: the gradual weakening of our bones. Yes, as the years pass, our once sturdy skeletal framework can become fragile, leaving us vulnerable to fractures and osteoporosis. But armed with knowledge and proactive steps, you can defy the odds and maintain robust bone health well into your golden years.
Understanding The Culprits: Why Do Bones Weaken with Age?
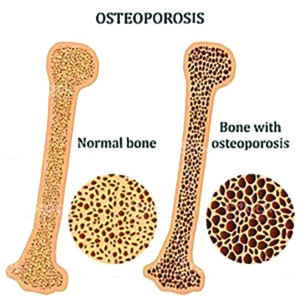
Bones are living tissues constantly undergoing a process of renewal. However, this renewal process can become less efficient as we age, leading to a decline in bone density and strength. Several factors contribute to this phenomenon:
Hormonal Changes: Hormones are pivotal in bone health, particularly estrogen and testosterone. As levels of these hormones decrease with age, bone density can decline, especially in postmenopausal women.
Nutritional Deficiencies: Adequate intake of calcium, vitamin D, and other essential nutrients is crucial for maintaining bone strength. Unfortunately, as dietary habits change over time or absorption becomes less efficient, deficiencies can arise, impacting bone health.
Physical Inactivity: Just as muscles weaken without exercise, bones also need regular physical activity to stay strong. Sedentary lifestyles accelerate bone loss, increasing the risk of fractures.
Genetic Factors: Family history plays a significant role in determining bone health. Individuals with a family history of osteoporosis or fractures may be predisposed to similar conditions.
Medical Conditions: Certain health conditions have been identified as potential catalysts for weakening bones and heightening the risk of osteoporosis. Among these are Rheumatoid Arthritis (RA), specific types of cancers, HIV/AIDS, anorexia nervosa, and various endocrine or gastrointestinal disorders. While these conditions impact individuals across all age groups, some, such as RA and certain cancers, tend to manifest more frequently as individuals age.
 Medications: According to the Bone Health and Osteoporosis Foundation (BHOF), certain medications have the potential to compromise bone strength, particularly when used over extended periods. These could include certain medications prescribed for acidity, seizures, cancer treatments, autoimmune disorders, managing acid reflux, managing Type-2 diabetes; blood thinners; steroids; and specific mental health conditions like bipolar disorder, depression and anxiety. Consult with your healthcare provider to check if you have been prescribed medications which impact your bone health. While the advantages of the medication may surpass potential risks to your bones, it’s essential to discuss alternative treatments or dosage adjustments to mitigate the risk of fractures in certain instances.
Medications: According to the Bone Health and Osteoporosis Foundation (BHOF), certain medications have the potential to compromise bone strength, particularly when used over extended periods. These could include certain medications prescribed for acidity, seizures, cancer treatments, autoimmune disorders, managing acid reflux, managing Type-2 diabetes; blood thinners; steroids; and specific mental health conditions like bipolar disorder, depression and anxiety. Consult with your healthcare provider to check if you have been prescribed medications which impact your bone health. While the advantages of the medication may surpass potential risks to your bones, it’s essential to discuss alternative treatments or dosage adjustments to mitigate the risk of fractures in certain instances.
Smoking / Drinking: Both – tobacco use and alcohol use, negatively affect bone health and make osteoporosis more likely.
5 Natural Methods To Maintain Bone Health With Age
While reversing time is beyond our grasp, there exist numerous strategies to uphold the resilience of your bones and naturally deter osteoporosis.
- Incorporate Calcium-Rich Foods In Your Diet: The majority of your body’s calcium is stored in your bones, making it crucial to consume sufficient calcium-rich foods to support bone health and strength. For adults under 50, the recommended daily intake of calcium is 600 milligrams; increasing to 800 (men) and 1200 milligrams (women) for those aged 50 and older. RDA (Recommended Dietary Allowance) during pregnancy differs with each trimester. Your body can absorb calcium from various sources including Milk or fortified soy milk, yoghurt, unprocessed cheese, dark leafy greens like kale or spinach, soybeans or edamame, calcium-fortified tofu and beans.
- Ensure Adequate Intake Of Other Bone-Healthy Nutrients: In addition to calcium, your body relies on various other nutrients, including vitamin D, vitamin K, potassium and magnesium, to promote robust bone development.
The most effective way to obtain these nutrients is by consuming a diverse range of nutrient-dense foods including fruits and vegetables, whole grains, lean proteins, nuts and beans.
III. Consult Your Doctor Regarding Supplementation: If you find it challenging to meet your calcium requirements through dietary sources alone, calcium supplements can serve as a helpful solution. However, it’s essential to discuss the advantages and disadvantages of supplementation with your healthcare provider, as a supplement may not offer the same benefits as a diet rich in calcium.
- Engage In Physical Activity: Engaging in activities that impose stress on your bones can mitigate bone density loss and promote the development of new bone tissue. These activities encompass walking, dancing, jogging, weightlifting, or participating in higher-impact sports like tennis or basketball. Remember, these activities primarily strengthen the bones directly involved. For eg., while walking and jogging benefits the bones in your lower body, they do not significantly impact the bones in your arms or wrists.
- Address Smoking And Moderate Alcohol Consumption: As previously highlighted, tobacco use and excessive alcohol consumption can detrimentally affect bone health. If you’re facing challenges in quitting smoking or alcohol consumption, consult your healthcare provider for assistance in overcoming smoking as a habit or limiting your alcohol intake.
Osteoporosis Screening
DEXA scan is a widely used method for osteoporosis screening. It assesses bone density levels, aiding in early detection and prevention of fractures. DEXA scans are non-invasive and offer precise measurements, enabling tailored treatment plans for individuals at risk of osteoporosis. DEXA scans are generally recommended for individuals aged 65 and older, particularly post-menopausal women and men over 70 years. However, screening may be advised earlier for individuals with specific risk factors or medical conditions predisposing them to osteoporosis. Consulting a healthcare provider helps determine the appropriate time for screening, based on individual circumstances.
When To See A Doctor?
Initiating discussions with your healthcare provider regarding bone health is essential, irrespective of age, particularly if you have a background of calcium or vitamin D insufficiency or have been prescribed medications that may jeopardize bone strength. If there’s a family history of osteoporosis or hip fractures, it’s advisable to commence these conversations as perimenopause approaches, typically occurring in one’s early or mid-40s. Build strong bones – start the conversation today!
- Healing or Harmful? - 15 March2025
- The Parsi Woman’s Guide To Superfoods For Hormonal Health - 8 March2025
- Strengthen Your Constitution This Republic Day! - 25 January2025
